The Centers for Disease Control and Prevention (CDC) has updated its "core elements" of hospital antibiotic stewardship programs.
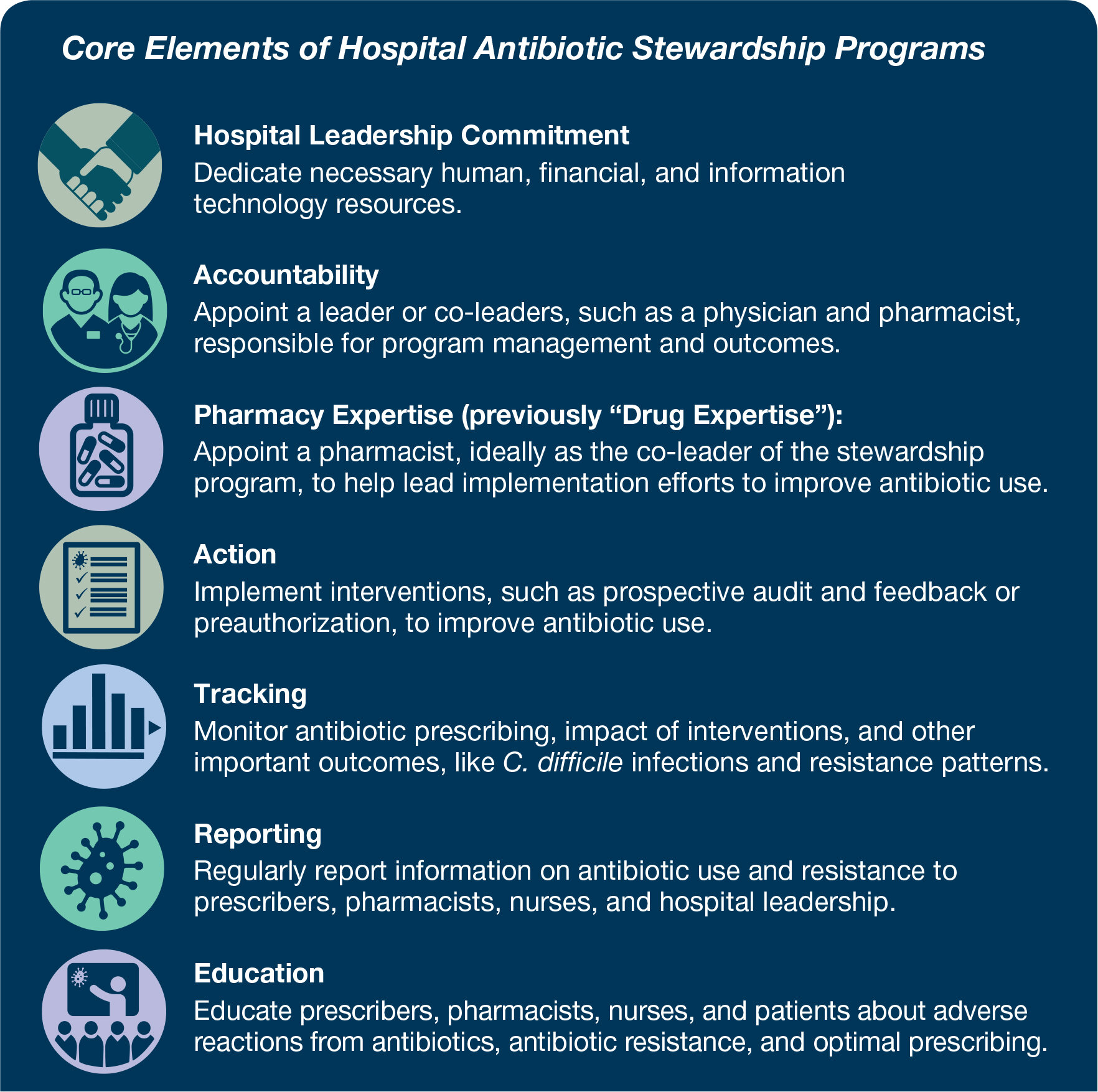
First released in 2014, the core elements are intended to be an adaptable framework that any hospital can use to guide its efforts to develop and implement antibiotic stewardship programs and help improve antibiotic prescribing. The core elements are comprised of seven structural and procedural components CDC has determined is associated with successful antibiotic stewardship programs: hospital leadership commitment, accountability, pharmacy expertise (formerly "drug expertise"), action, tracking, reporting and education.
CDC said its updates "reflect both lessons learned from five years of experience as well as new evidence from the field of antibiotic stewardship."
Major updates include the following:
Hospital leadership commitment: Dedicate necessary human, financial and information technology resources. This includes hospital leadership better ensuring that antibiotic stewardship programs leadership has dedicated time and resources to operate the program effectively, along with ensuring that program leadership has regularly scheduled opportunities to report stewardship activities, resources and outcomes to hospital leadership.
Accountability: Appoint a leader or co-leaders, such as a physician and pharmacist, responsible for program management and outcomes.
Pharmacy expertise: Appoint a pharmacist, ideally as the co-leader of the stewardship program, to lead implementation efforts to improve antibiotic use.
Action: Implement interventions, such as prospective audit and feedback or preauthorization, to improve antibiotic use. The update includes other examples of interventions, such as facility-specific treatment recommendations. The update also emphasizes the importance of actions focused on the most common indications for hospital antibiotic use (i.e., lower respiratory tract infection (e.g., community-acquired pneumonia), urinary tract infection and skin and soft tissue infection). A category of nursing-based actions was added in the update.
Tracking: Monitor antibiotic prescribing, impact of interventions and other important outcomes like Clostridium difficile infection and resistance patterns.
Reporting: Regularly report information on antibiotic use and resistance to prescribers, pharmacists, nurses and hospital leadership.
Education: Educate prescribers, pharmacists and nurses about adverse reactions from antibiotics, antibiotic resistance and optimal prescribing. The update notes that case-based education through prospective audit and feedback and preauthorization are effective methods to provide education on antibiotic use. The update also suggests engaging nurses in patient education efforts.
As CDC notes, U.S. hospitals have made considerable progress implementing the core elements. In 2018, 85% of acute care hospitals reported having all seven of the core elements in place, compared to only 41% in 2014.
For more information about the update, download "The Core Elements of Hospital Antibiotic Stewardship Programs: 2019" and watch a CDC-produced video discussing what's new in the core elements.